# New Insights on Vaccination: More Shots, More Infections, Yet Less Severe Covid
Written on
Understanding the Paradox of Vaccination
Recent research has unveiled a perplexing trend in Covid-19 vaccinations: a rise in infections correlating with more vaccine doses, yet with less severe outcomes. Factors such as group behavior, immune imprinting, and the IgG4 class switch are believed to play significant roles.

A recent and bold study from the Cleveland Clinic, a distinguished non-profit medical center, has produced concerning data indicating that increased vaccine doses might elevate the risk of contracting Covid-19 (see Figure 1):
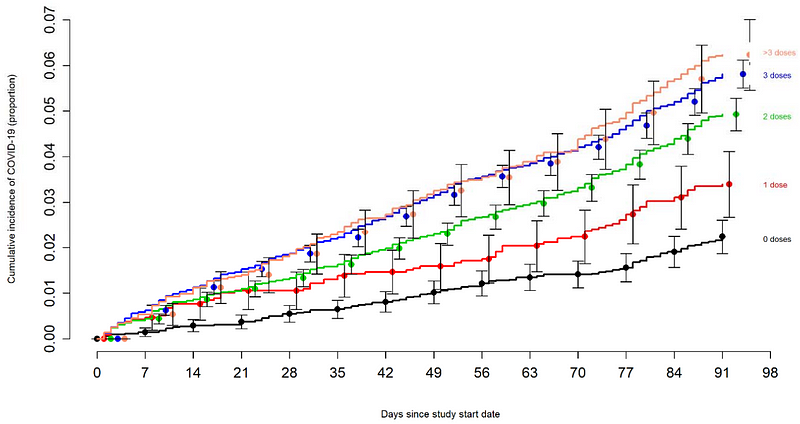
Figure 1. A comparison of Covid-19 incidence among individuals based on their total number of vaccine doses, with the starting point marked as September 12, 2022, the day the bivalent vaccine was made available to staff. Source: Shrestha et al. (2022).
As is often the case, this data has been interpreted by some as evidence that receiving multiple vaccinations may diminish immunity against Covid. While the graph certainly supports this view, it is crucial to consider additional factors before drawing any definitive conclusions regarding the data.
Current Insights on Booster Efficacy
In the study conducted by Shrestha et al., researchers examined the effectiveness of the bivalent mRNA vaccine, which targets both the Omicron BA.1/2 variants and the original Wuhan strain of SARS-CoV-2. Although mRNA vaccines had previously demonstrated efficacy in clinical trials, the bivalent mRNA vaccines received approval without new trials, requiring only safety data.
The team engaged 51,011 participants (average age of 42 years, with 41% having had prior Covid, and 87% having received at least one vaccine dose) from the Cleveland Clinic. Among them, around 21% (10,804 individuals) received the bivalent mRNA vaccine (89% from Pfizer and 11% from Moderna), while 5% (2,452 individuals) contracted Covid.
After controlling for age, gender, previous vaccination doses, and other variables, the bivalent mRNA vaccine was found to reduce the risk of Covid by 30%. However, the authors noted an alarming trend: “the greater the number of vaccine doses previously received, the higher the risk of COVID-19” (see Figure 1).
Notably, other cohort studies have echoed these findings. A nationwide investigation from Qatar reported a 38% increased risk of Omicron reinfection (likely BA.4/5) among triple-vaccinated individuals compared to those who had received only two doses. However, both the double- and triple-vaccinated groups still exhibited a 57% and 47% reduced risk of reinfection, respectively, relative to unvaccinated individuals. Fortunately, none of the reinfection cases were severe.
Similarly, another significant study from the Cleveland Clinic indicated that individuals with 2–3 doses of mRNA vaccine faced a 54% higher risk of reinfection (likely BA.4/5) when compared to those with just one dose.
While one study from the Netherlands suggested that booster shots provide a 58–68% protection against Omicron BA.1 infection, it focused on earlier variants and was published prior to the emergence of more immune-evasive strains.
Nevertheless, mRNA vaccine boosters continue to offer protection against severe Covid outcomes, particularly among older populations. For instance, a recent preprint from Israel revealed that seniors aged 65 and older who received the bivalent mRNA booster experienced an 81% and 86% reduction in the risk of hospitalization and death due to Covid compared to those who only received 2–3 doses of the monovalent mRNA vaccine (see Figure 2).
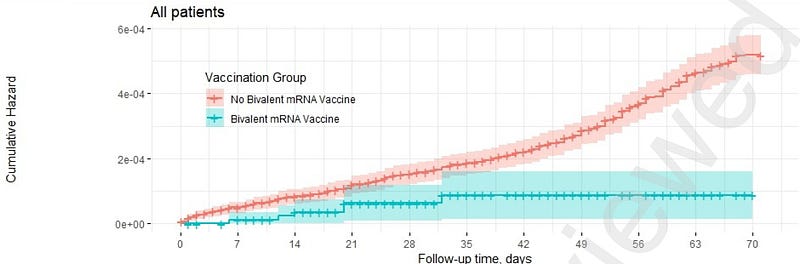
Figure 2. Comparison of hospitalization rates for Covid-19 between recipients of the bivalent mRNA booster (cyan) and those who received only monovalent mRNA vaccines (red). Source: Arbel et al. (2023).
Recent data from the CDC corroborates these findings, showing that the bivalent mRNA booster reduces hospitalization risk by 57% compared to unvaccinated individuals and 38–45% compared to monovalent vaccination among adults aged 18 and above. This protective effect is even more pronounced in older adults (≥65 years), with a 73% reduction in risk compared to those receiving only monovalent vaccinations.
While the Israel and CDC studies did not specifically analyze the bivalent booster’s effectiveness against Covid infection, the previous cohort studies suggest limited benefits.
Deciphering Increased Infections with Reduced Severity
To understand the paradox of rising infections alongside diminished disease severity following multiple vaccinations, three primary factors must be considered: group behavior, immune imprinting, and IgG4 class switching.
Part I: Group Behavioral Variances
It is essential to note that all these cohort studies are observational, inherently lacking the ability to establish cause-and-effect relationships due to potential biases. For instance, Shrestha et al. recognized that “Individuals who opted for the bivalent vaccine may have been more concerned about infection, potentially leading them to seek testing when symptomatic, thus skewing the infection rates among vaccinated individuals.”
They also pointed out that “If individuals believed the bivalent vaccine would lower their infection risk, they might have been less inclined to undergo testing.”
This highlights the "healthy vaccinee effect," where those in poorer health are less likely to receive vaccinations, resulting in skewed outcomes in unvaccinated or less vaccinated groups—a significant confounding variable in observational vaccine studies.
Moreover, correlation does not imply causation. For example, severe Covid has been associated with corticosteroid use, but this is due to corticosteroids being utilized in treating severe cases rather than causing them. Similarly, ice cream sales may correlate with shark attacks due to seasonal behavior rather than a direct relationship.
Shrestha et al. stated, “The association of increased risk of COVID-19 with higher numbers of prior vaccine doses in our study was unexpected. A simplistic explanation could be that those who received more doses were inherently at greater risk of COVID-19.”
However, the protective nature of mRNA vaccine boosters against severe Covid implies that testing frequency is less relevant in assessing outcomes, as severe cases will manifest in hospitals regardless of testing rates.
Part II: Immune Imprinting
Another potential explanation for the rise in Covid infections with more vaccinations could be immune imprinting (also referred to as original antigenic sin). This possibility, while not discussed by the authors, merits consideration.
Immune imprinting occurs when older antibodies, generated in response to previous variants, are activated against newer variants. These outdated antibodies are often ineffective and might even hinder the development of more effective antibodies. Essentially, the immune system continues to rely on its initial training, failing to adapt to new challenges.
This phenomenon has been observed with various vaccines. For instance, seasonal flu vaccines typically have an effectiveness of only 40%–60%, partly due to immune imprinting interfering with newer vaccine responses.
Similarly, research has indicated that individuals previously vaccinated against HPV exhibited weaker immune responses to updated HPV vaccines compared to those who had never been vaccinated.
In the context of Covid vaccines, a study published in Science found that triple-vaccinated individuals infected with Omicron displayed lower antibody and T-cell responses than those who had never been infected. Another study indicated that over 80% of antibodies in Omicron breakthrough cases reacted with older strains of SARS-CoV-2, while unvaccinated, never-infected individuals had more Omicron-specific antibodies.
The authors of the Qatar study remarked that their findings “suggest that the immune response against initial Omicron infection was compromised by differential immune imprinting in those who received a third booster dose, consistent with emerging laboratory science data.”
Despite the presence of non-specific antibodies due to immune imprinting, these antibodies may still be deployed more rapidly in vaccinated individuals, potentially mitigating disease severity.
Part III: IgG4 Class Switching
Another potential factor for the increased risk of Covid infections among those who have received multiple vaccinations is the IgG4 class switch, which occurs 3–7 months after the second dose and remains present for several months following the third dose of the mRNA vaccine.
Unlike immune imprinting, the IgG4 class switch has only recently come to light, and its implications have been discussed in previous literature.
In summary, immunoglobulins (IgG) consist of four subclasses: IgG1, IgG2, IgG3, and IgG4. IgG1 and IgG3 are pro-inflammatory and primarily responsible for driving antibody-dependent immune responses, while IgG2 and IgG4 are less effective in this regard but serve as anti-inflammatory agents.
A significant study from Germany revealed that individuals with repeated mRNA vaccinations initially exhibited high levels of IgG1 and IgG3, but after several months, IgG4 levels began to rise, indicating an IgG4 class switch. This shift was associated with reduced phagocytic and complement activation activities, raising concerns about vaccine effectiveness.
Phagocytosis involves immune cells ingesting foreign materials, including virus-infected cells, while the complement system enhances various immune functions.
This data can be interpreted in two ways:
- The IgG4 class switch may weaken antibody-dependent responses, contributing to increased infections.
- The IgG4 class switch may serve as a regulatory mechanism to limit inflammation, potentially resulting in improved disease outcomes.
The first scenario might explain the correlation observed in extensive cohort studies, indicating that more vaccinations lead to higher risks of Omicron infections. The second scenario could clarify why those with more vaccinations experience better clinical outcomes.
Making Sense of the Findings
Overall, current observational studies indicate that while increased mRNA vaccinations may correlate with a higher risk of Omicron infections and reinfections, the severity of Covid illness remains lower, particularly among older adults.
This complex situation likely arises from a combination of factors, including group behavior, immune imprinting, and the IgG4 class switch.
Understanding vaccine effectiveness requires a nuanced approach, as underlying factors may not be immediately apparent.
Implications for the Risk-Benefit Balance of Covid Vaccines
Dr. Paul A. Offit, a prominent expert in vaccinology and pediatrics, articulated a critical perspective on this topic in a 2023 article in The New England Journal of Medicine:
“…booster doses are likely best reserved for those most at risk for severe disease — specifically, older adults, individuals with multiple health conditions, and those who are immunocompromised.”
He further suggested that efforts to prevent all symptomatic infections in healthy young individuals through repeated mRNA vaccinations may be misguided, especially given the rapidly changing nature of viral strains.
In summary, individuals at low risk for severe Covid may derive minimal benefit from receiving additional mRNA vaccinations, as the potential risks — such as myocarditis, POTS, and immune imprinting — may outweigh the advantages. Furthermore, Omicron tends to be less severe and poses a lower risk of long-term complications than earlier variants, with effective treatments available for Covid.
Consequently, beyond the initial 2–3 doses, it is challenging to justify further vaccinations for healthy individuals based on the current evidence.
Thank you for your attention. For more insights, consider subscribing to my Medium email list. If you're interested in accessing unlimited content on Medium, feel free to use my referral link, which provides me with a small commission at no extra cost to you. Your support is greatly appreciated!