The Truth About Vitamin D and COVID-19: Myths and Realities
Written on
Chapter 1: Understanding Vitamin D's Controversial Role
Vitamin D has sparked a significant amount of debate. If you've ever delved into discussions about this vital nutrient, you may have noticed how fervently people defend it, much like sports fans rally around their teams. The claims surrounding vitamin D range from its ability to cure heart disease to its potential in combating cancer, leading to an abundance of studies on this vitamin, more than nearly any other supplement found in the health aisle of your local grocery store.

As with many popular health supplements, the claims often exceed reality. Throughout the COVID-19 pandemic, various individuals have touted vitamin D as an effective treatment, often referencing questionable and occasionally fabricated research. While the highest quality studies generally show minimal benefits from vitamin D supplementation, the lack of robust trials makes it difficult to draw definitive conclusions.
Recently, a viral notion has circulated online suggesting that vitamin D could completely eradicate the risk of dying from COVID-19. This claim raises eyebrows since rigorous randomized trials have consistently failed to demonstrate any mortality benefits associated with vitamin D supplementation. How, then, could it possibly bring your risk down to zero?
The truth is, this assertion is likely unfounded. While taking vitamin D may be beneficial, it will not completely eliminate your risk of contracting or dying from COVID-19.
Bad Science
A recent review paper published in the journal Nutrients examined observational studies linking vitamin D levels and mortality. The authors compiled findings from seven hospital studies and one ecological study that assessed population-level vitamin D data, finding a weak correlation between vitamin D levels and COVID-19 mortality.
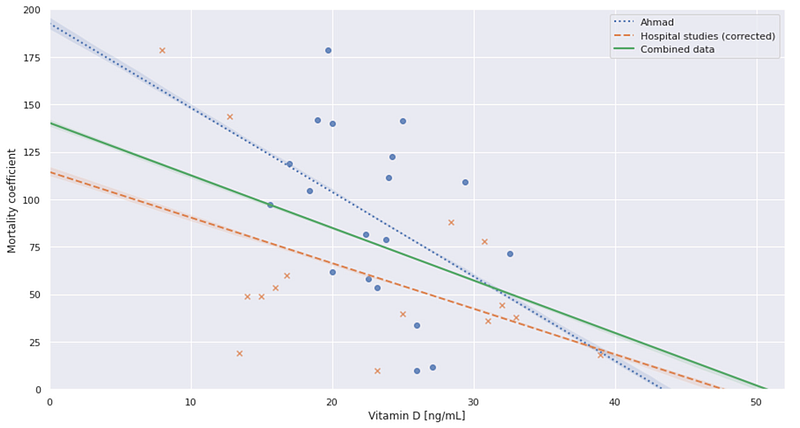
Using this regression analysis, the authors claimed that at a certain level of vitamin D (50.7 ng/mL), there could theoretically be zero mortality. However, numerous flaws undermine this conclusion. First, the review relies heavily on low-quality research studies. The ecological trial, for instance, sourced its vitamin D data from a study dating back to 1992, which is hardly a reliable measure of current vitamin D levels.
Furthermore, many observational studies included in the review are quite small, some involving as few as 29 participants. These limited sample sizes hinder any meaningful understanding of the relationship between vitamin D levels and mortality rates. Additionally, most studies failed to adjust for confounding variables, leaving open the question of whether low vitamin D levels are a cause or simply a byproduct of severe illness.
The review's methodology is also questionable. Though labeled a systematic review, it lacks comprehensive coverage of relevant studies, indicating a significant oversight in the selection process.
Moreover, the linear regression analysis is fundamentally flawed. The studies often provided average vitamin D values rather than specific data points, making the analysis less reliable. The idea that a regression line intersecting zero at 50 ng/mL could imply a "theoretical point of zero mortality" is a gross misinterpretation of statistical principles.
This kind of extrapolation from regression data is misleading and misinformed. For instance, if one were to maintain a vitamin D level of 60 ng/mL, does that imply a negative risk of COVID-19 mortality? Such reasoning is nonsensical. A closer examination of the data reveals that most population averages often exceed 50 ng/mL, yet the studies reviewed primarily focused on hospitalized patients, skewing the data and rendering it irrelevant for the general population.
Conclusion
Ultimately, the study in question is rife with inconsistencies and should not be considered credible evidence for any claims regarding vitamin D and COVID-19. The research merely aggregates various inconclusive studies, presenting vague correlations without substantial backing.
We find ourselves in a similar situation to when I last discussed vitamin D's potential role in COVID-19 back in early 2021: while there may be some plausible benefits to supplementation, the current evidence remains inadequate. A recent systematic review indicates that only one well-conducted randomized trial has examined vitamin D supplementation's impact on COVID-19, and it found no significant benefits.
As I stated previously and will likely reiterate in the future as the hype resurfaces, you can choose to take vitamin D supplements if you wish. They are generally safe, albeit with some risks, but are unlikely to eliminate your vulnerability to COVID-19. Vitamin D is indeed beneficial, yet relying on supplementation as a cure-all for anything, particularly COVID-19, is not supported by the high-quality evidence available.
Chapter 2: Video Insights on Vitamin D and COVID-19
This video titled "The Vitamin D Paradox in COVID-19: Why It Predicts But Doesn't Always Protect" delves into the complex relationship between vitamin D levels and COVID-19 outcomes, highlighting the paradoxical evidence that suggests benefits without guarantees.
Another insightful video, "Vitamin D and COVID-19: The Evidence for Prevention and Treatment of Coronavirus (SARS CoV 2)," explores the existing research surrounding vitamin D's role in preventing and treating COVID-19, offering a comprehensive overview of the topic.