Innovative Cancer Treatments: CAR-T Therapy and Its Impact
Written on
Introduction to CAR-T Therapy
Recent advancements in cancer treatment have been notable, even amidst the challenges posed by the COVID-19 pandemic. Various innovative therapies have emerged, including cancer vaccines and promising technologies for targeting cancer metastasis. One of the most groundbreaking developments is the CAR-T therapy, which has demonstrated remarkable success in keeping cancer at bay for over ten years in some patients.
The Journey of CAR-T Therapy
Administered to select patients in 2010, CAR-T therapy has yielded impressive results. Scientists Carl June and David Porter from the University of Pennsylvania were initially optimistic but cautious, as they anticipated the genetically modified T-cells might only survive for about a month. However, they were taken aback by the outcome: weeks after treatment, one patient showed no traces of cancer cells in their system.
Despite this early success, long-term outcomes remained uncertain. Fast forward a decade, and that same leukemia patient continues to thrive, with immune cells actively maintaining the remission state.
Understanding CAR-T Mechanism
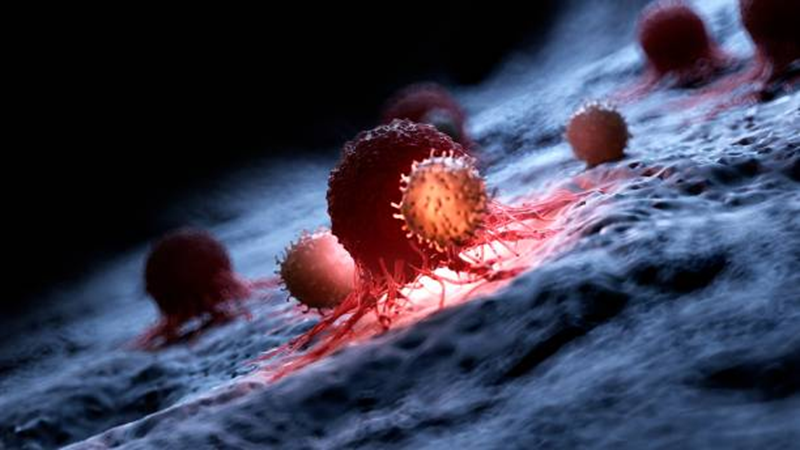
To grasp how CAR-T therapy operates, it’s essential to note that it involves genetically modifying T-cells harvested from patients. This modification allows the T-cells to produce chimeric antigen receptors (CARs), enabling them to detect and eliminate cancerous cells. Once these modified cells are reintroduced into the patient, they effectively target tumors.

Expert Insights on CAR-T Therapy
“The potential impact of CAR-T is tremendous… it provides proof of concept regarding the safety and long-term integration of T-cells in the human body.”
~ Nirali Shah, US National Cancer Institute

Regulatory Approval and Challenges
Since the initial CAR-T treatments, the US Food and Drug Administration (FDA) has approved five therapies for leukemias, lymphomas, and myelomas, benefiting thousands of patients. However, CAR-T therapy is costly and complicated, making it suitable primarily when other treatment avenues have failed.
Research indicates that only 25-35% of chronic lymphocytic leukemia patients initially achieved complete remission with CAR-T therapy. Nevertheless, ongoing refinements in the treatment have improved success rates, and long-term studies are crucial to uncovering insights for sustained efficacy.
Evolution of CAR-T Cells
Over the years, researchers have monitored the evolution of CAR-T cells in patients. They observed that while CAR-T cells persisted, their characteristics changed. The infusion resulted in the emergence of CD8+ killer T cells, capable of targeting and destroying cancerous and virally infected cells. Interestingly, another type of CAR-T cell, CD4+, also became prominent, contributing significantly to the immune response against leukemia.
Future Directions in Cancer Treatment
Encouraged by their findings, researchers are now aiming to apply CAR-T therapy to solid tumors, such as those found in prostate cancer and glioblastoma. Recently, innovative techniques have been explored to utilize this approach for addressing scar tissue in cardiac patients, potentially paving the way for treating cardiac fibrosis.
With these promising developments, the hope for effective and enduring cancer treatments appears closer than ever.
Complete Research published in the Journal of Nature.
The first video presents a breakthrough in cancer treatment through AI and immunotherapy, showcasing the transformative potential of these technologies.
The second video highlights CAR-T cell therapy, illustrating how it brings new hope to cancer patients through innovative approaches.